Top Stories
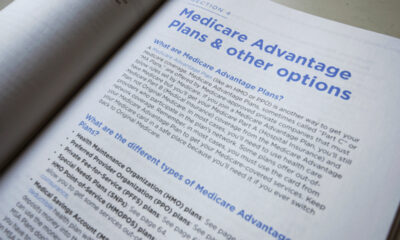
Medicare Launches Urgent AI Pilot Program to Review Care Requests

UPDATE: Medicare just announced a groundbreaking pilot program allowing private companies to utilize artificial intelligence (AI) for reviewing medical care requests from older Americans. This initiative, termed the Wasteful and Inappropriate Services Reduction (WISeR) Model, will reward these companies for denying care, raising significant concerns among healthcare advocates and physicians.
Beginning in January 2024, the Centers for Medicare & Medicaid Services (CMS) will implement this program across six states: Arizona, New Jersey, Ohio, Oklahoma, Texas, and Washington. The pilot is set to run until 2031, effectively introducing prior authorization—a common feature criticized in private insurance—into traditional Medicare, which serves individuals aged 65 and older.
This new approach mandates that Medicare patients and their doctors seek approval from insurance companies before proceeding with certain medical procedures or prescriptions. The services targeted include knee arthroscopy for osteoarthritis, incontinence control devices, and specific nerve stimulation treatments, all identified as vulnerable to fraud and waste.
Physicians and patient advocates have expressed alarm over the potential consequences of this AI-driven model. Dr. Bindu Nayak, an endocrinologist in Washington, highlighted the risks for Medicare recipients, stating, “The WISeR program puts more barriers up for them accessing care. They may have to deal with prior authorization when they never had to before.”
“Prior authorization delays care and sometimes denies treatment to patients who need it,” said Dr. Jayesh Shah, president of the Texas Medical Association.
Critics argue the program could exacerbate existing issues with prior authorization, which has been linked to serious health consequences, including hospitalization. According to the American Medical Association, more than a quarter of physicians reported that prior authorization issues led to significant problems for their patients.
CMS’s initiative is controversial, particularly as it introduces financial incentives for companies that save Medicare money by denying care. The agency’s strategy aims to cut costs, with Medicare having spent up to $5.8 billion in 2022 on services deemed to have minimal benefit to patients.
In response to the announcement, U.S. Representative Suzan DelBene (D-WA) and other lawmakers have introduced a bill aiming to repeal the WISeR model, citing concerns over its potential to hinder access to necessary care for seniors. “The administration has publicly admitted prior authorization is harmful, yet it is moving forward with this misguided effort,” DelBene stated.
As the pilot program prepares for launch, stakeholders remain alert to its implications. With bipartisan concerns over prior authorization growing, many fear the added administrative burden will lead to longer wait times and increased denials for patients seeking care. “Patients may face more barriers in the form of denials, but they should continue to advocate for themselves,” Dr. Nayak emphasized.
As the January start date approaches, the healthcare community is watching closely to see how the WISeR model will unfold and its potential impact on the lives of millions of Medicare patients across the nation.
-

 Top Stories1 month ago
Top Stories1 month agoUrgent Update: Tom Aspinall’s Vision Deteriorates After UFC 321
-

 Science1 month ago
Science1 month agoUniversity of Hawaiʻi Joins $25.6M AI Project to Enhance Disaster Monitoring
-
 Health2 months ago
Health2 months agoMIT Scientists Uncover Surprising Genomic Loops During Cell Division
-

 Top Stories2 months ago
Top Stories2 months agoAI Disruption: AWS Faces Threat as Startups Shift Cloud Focus
-
 Science2 months ago
Science2 months agoTime Crystals Revolutionize Quantum Computing Potential
-

 Entertainment2 months ago
Entertainment2 months agoDiscover the Full Map of Pokémon Legends: Z-A’s Lumiose City
-

 Entertainment2 months ago
Entertainment2 months agoParenthood Set to Depart Hulu: What Fans Need to Know
-

 Top Stories2 months ago
Top Stories2 months agoGOP Faces Backlash as Protests Surge Against Trump Policies
-

 World2 months ago
World2 months agoHoneywell Forecasts Record Business Jet Deliveries Over Next Decade
-

 Politics2 months ago
Politics2 months agoJudge Signals Dismissal of Chelsea Housing Case Citing AI Flaws
-
 Health2 months ago
Health2 months agoMaine Insurers Cut Medicare Advantage Plans Amid Cost Pressures
-

 Sports2 months ago
Sports2 months agoYoshinobu Yamamoto Shines in Game 2, Leading Dodgers to Victory









