Health
New Study Links Combined Cholesterol and Inflammation Markers to Heart Risk

A recent study has established that a combined measurement of LDL cholesterol, high-sensitivity C-reactive protein (hsCRP), and lipoprotein(a) [Lp(a)] can effectively predict major adverse cardiovascular events (MACE) among initially healthy individuals over a span of 20 years. This research, part of the EPIC-Norfolk study conducted in the United Kingdom, aims to validate findings from a previous American trial that examined nearly 28,000 healthy women over three decades.
The earlier study revealed a significant correlation between the combination of hsCRP, LDL, and Lp(a) and the occurrence of cardiovascular events. Researchers, including lead author Jordan Kraaijenhof from the Amsterdam Cardiovascular Sciences, highlighted the necessity for universal screening in primary prevention, echoing recommendations from the Women’s Health Study (WHS). Kraaijenhof stated, “We sought to determine whether the predictive value of LDL cholesterol, hsCRP, and Lp(a), both individually and in combination, extends to a European primary prevention population.”
To investigate this, Kraaijenhof and his team recruited 17,087 participants aged 40 to 79 from general practices in Norfolk, UK. Each participant completed comprehensive health and lifestyle questionnaires, with further data collected by trained nurses during clinic visits. Non-fasting blood samples were obtained to measure plasma levels of total cholesterol, HDL cholesterol, and triglycerides, while LDL cholesterol levels were calculated. Additionally, hsCRP levels were analyzed from frozen serum samples, and Lp(a) concentrations were measured using an isoform-independent immunoturbidimetric assay.
The primary aim of the study was to evaluate the relationship between LDL cholesterol, hsCRP, and Lp(a) in predicting cardiovascular risk. Each biomarker was assessed independently before evaluating their combined impact on cardiovascular events. MACE was defined as either fatal or non-fatal coronary artery disease and fatal or non-fatal ischemic stroke. Investigators documented MACEs during follow-ups, which included instances where participants were hospitalized or died from coronary artery disease or ischemic stroke as the primary cause.
Participants had a mean age of 59 years, with baseline levels of LDL cholesterol averaging 4 +/- 1 mmol/L, hsCRP at 1.5 (0.7-3.2) mg/L, and Lp(a) at 11 (6-27) mg/dL. The follow-up period lasted a median of 20.5 years. Throughout this time, researchers recorded 3,249 first MACEs, which included 1,755 events among female participants and 1,494 among male participants.
The study analyzed the age- and sex-adjusted hazard ratios (HRs) for MACE, contrasting the highest and lowest quintiles. The results indicated an HR of 1.84 (95% CI, 1.64-2.08) for LDL, 1.75 (95% CI, 1.56-1.97) for hsCRP, and 1.28 (95% CI, 1.15-1.42) for Lp(a). Multivariable-adjusted HRs for each quintile increase were 1.14 (95% CI, 1.11-1.17) for LDL, 1.12 (95% CI, 1.09-1.15) for hsCRP, and 1.05 (95% CI, 1.02-1.08) for Lp(a). The combination of all three biomarkers in their highest quintiles posed the greatest risk for MACE.
Kraaijenhof and his colleagues concluded, “These data both replicate and extend very recent American evidence that a simple biomarker panel can detect unique patterns of risk for many patients that would otherwise be missed using traditional global risk algorithms or commonly used imaging tests.” They emphasized that commercial assays for hsCRP and Lp(a) are standardized, affordable, and widely accessible. The authors advocate for the implementation of universal screening for these three biomarkers in both primary and secondary prevention of cardiovascular disease.
-

 Top Stories1 month ago
Top Stories1 month agoUrgent Update: Tom Aspinall’s Vision Deteriorates After UFC 321
-
 Health1 month ago
Health1 month agoMIT Scientists Uncover Surprising Genomic Loops During Cell Division
-

 Science4 weeks ago
Science4 weeks agoUniversity of Hawaiʻi Joins $25.6M AI Project to Enhance Disaster Monitoring
-

 Top Stories1 month ago
Top Stories1 month agoAI Disruption: AWS Faces Threat as Startups Shift Cloud Focus
-
 Science2 months ago
Science2 months agoTime Crystals Revolutionize Quantum Computing Potential
-

 World2 months ago
World2 months agoHoneywell Forecasts Record Business Jet Deliveries Over Next Decade
-

 Entertainment1 month ago
Entertainment1 month agoDiscover the Full Map of Pokémon Legends: Z-A’s Lumiose City
-

 Top Stories2 months ago
Top Stories2 months agoGOP Faces Backlash as Protests Surge Against Trump Policies
-

 Entertainment2 months ago
Entertainment2 months agoParenthood Set to Depart Hulu: What Fans Need to Know
-

 Politics2 months ago
Politics2 months agoJudge Signals Dismissal of Chelsea Housing Case Citing AI Flaws
-

 Sports2 months ago
Sports2 months agoYoshinobu Yamamoto Shines in Game 2, Leading Dodgers to Victory
-
 Health2 months ago
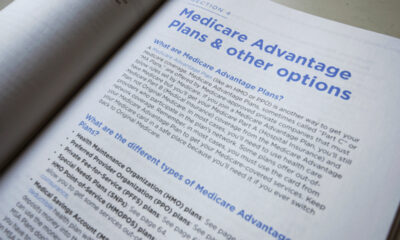
Health2 months agoMaine Insurers Cut Medicare Advantage Plans Amid Cost Pressures







