Health
FDA Eases Hormone Therapy Warnings, Igniting Controversy Among Experts

The US Food and Drug Administration (FDA) announced a significant change last week, removing broad black-box warnings related to menopause hormone therapy, a decision that has sparked intense debate among medical professionals. According to Marty Makary, FDA commissioner, this move is a step towards recognizing the potential benefits of hormone replacement therapy (HRT) for women undergoing menopause.
The agency’s decision eliminates a warning established in 2003 that linked systemic estrogen treatments to risks such as cardiovascular disease, breast cancer, and dementia. While local vaginal estrogen products may be less contentious, experts argue that the implications for systemic estrogen are more complex. Critics claim that the FDA’s choice to bypass traditional regulatory processes raises concerns about the scientific integrity of the decision-making.
Hormone therapy has been shown to alleviate common menopause symptoms, including hot flashes and insomnia. Makary emphasized the treatment’s broader implications, stating that it could potentially prevent serious health issues like heart disease and osteoporosis. He described HRT as a “life-changing, even life-saving treatment,” framing the announcement as a breakthrough for women’s health.
Others, such as Robert F Kennedy Jr., secretary of the US Department of Health and Human Services (HHS), expressed optimism, suggesting that hormone therapy could extend women’s lives by up to ten years. Similarly, Alicia Jackson, head of the Advanced Research Projects Agency for Health, stated that estrogen represents one of the most effective longevity interventions for women.
Despite these bold claims, many researchers caution against generalizing the benefits of hormone therapy. Lauren Streicher, clinical professor of obstetrics and gynecology at Northwestern University, criticized the broad assertion that all women should consider HRT to prevent heart disease, calling it unfounded. She expressed concern that the FDA’s decision sends a “harmful” and misleading message to women seeking clear information about their health options.
The controversy is compounded by the fact that the FDA relied on a roundtable panel, which did not allow for public comment before making its recommendations. Streicher, who initially planned to participate in the panel, withdrew after realizing it would not adhere to scientific rigor. She described the atmosphere at the press conference as orchestrated, with organizers encouraging attendees to wear white coats to lend an air of credibility to the event.
The lack of oncologists on the panel has also drawn criticism. The panel consisted of researchers and popular social media doctors, which Streicher described as potentially skewing the decision-making process. Makary defended the choice, remarking that traditional advisory committee meetings can be lengthy and fraught with conflicts.
The evidence surrounding hormone therapy remains nuanced. Streicher noted that local vaginal estrogen products are generally safe and effective for treating specific symptoms. However, systemic estrogen treatments involve various formulations that can present risks, such as an increased likelihood of blood clots. She advocated for a more tailored approach to labeling these products based on their specific risks and benefits.
Research conducted by Pauline Maki, a professor at the University of Illinois, has revealed troubling trends regarding hormone therapy’s effects on memory and cognition. Maki’s studies indicated that, contrary to earlier beliefs, hormone therapy does not show benefits for memory among the broader population of menopausal women. In fact, her randomized trials suggested a trend toward harm when hormone therapy was used for dementia prevention.
Despite this, health officials have downplayed the risks, citing a small study that suggested benefits for women who start HRT within ten years of menopause. Maki criticized the decision as cherry-picking data and emphasized the need for a more comprehensive examination of the available evidence.
Makary’s decision has drawn attention not only for its potential impact on women’s health but also for its implications for regulatory processes. The FDA’s approach has raised questions about the future of drug safety evaluations, with Makary indicating that more panels featuring passionate voices will influence future decisions.
The FDA’s decision to remove the black-box warnings has been framed by some as a challenge to established medical norms. Kennedy stated that the previous labels were designed to instill fear rather than inform, claiming that the American medical community had failed to advocate for women’s health.
While the FDA aims to reposition hormone therapy as a viable option for many women, experts like Streicher advocate for a cautious approach. She reiterated that while hormone therapy is effective for women experiencing significant menopause symptoms, it is not a blanket solution for all women undergoing the transition.
As the debate unfolds, the implications of the FDA’s decision will likely continue to resonate within the medical community and among women navigating menopause. The balance between providing effective treatments and ensuring rigorous scientific scrutiny remains a critical conversation in women’s health.
-

 Top Stories1 month ago
Top Stories1 month agoUrgent Update: Tom Aspinall’s Vision Deteriorates After UFC 321
-
 Health1 month ago
Health1 month agoMIT Scientists Uncover Surprising Genomic Loops During Cell Division
-

 Science4 weeks ago
Science4 weeks agoUniversity of Hawaiʻi Joins $25.6M AI Project to Enhance Disaster Monitoring
-

 Top Stories1 month ago
Top Stories1 month agoAI Disruption: AWS Faces Threat as Startups Shift Cloud Focus
-
 Science2 months ago
Science2 months agoTime Crystals Revolutionize Quantum Computing Potential
-

 World2 months ago
World2 months agoHoneywell Forecasts Record Business Jet Deliveries Over Next Decade
-

 Entertainment1 month ago
Entertainment1 month agoDiscover the Full Map of Pokémon Legends: Z-A’s Lumiose City
-

 Top Stories2 months ago
Top Stories2 months agoGOP Faces Backlash as Protests Surge Against Trump Policies
-

 Entertainment2 months ago
Entertainment2 months agoParenthood Set to Depart Hulu: What Fans Need to Know
-

 Politics2 months ago
Politics2 months agoJudge Signals Dismissal of Chelsea Housing Case Citing AI Flaws
-

 Sports2 months ago
Sports2 months agoYoshinobu Yamamoto Shines in Game 2, Leading Dodgers to Victory
-
 Health2 months ago
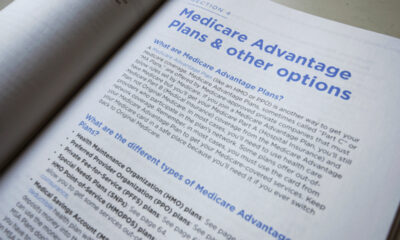
Health2 months agoMaine Insurers Cut Medicare Advantage Plans Amid Cost Pressures









