Health
Researchers Discover Gut-Brain Connection Limits Protein Intake

A recent study published in the journal Cell reveals a significant gut-to-brain signaling pathway that restricts protein appetite during recovery from illness. Researchers at Yale School of Medicine, led by Dr. Nikolai Jaschke and Dr. Andrew Wang, uncovered this mechanism while investigating why patients often experience decreased appetite for protein-rich foods after acute illnesses.
Dr. Jaschke, who has transitioned to a principal investigator role at the Hamburg Center for Translational Immunology in Germany, expressed concern over the lack of therapeutic support for individuals feeling unwell post-illness. “While this is common, there’s no real way to quantify what’s going on,” he stated. The team aimed to explore the physiological changes occurring during recovery, specifically focusing on appetite regulation.
Link Between Illness and Protein Appetite
Many individuals experience a reduced appetite when ill, leading to a catabolic state where the body breaks down proteins for energy. To investigate this phenomenon, the researchers conducted experiments with mice in a catabolic state, offering them diets high in protein, carbohydrates, or fats. The findings were striking; mice that were provided a protein-rich diet consumed significantly less food compared to those not in a catabolic state.
The researchers delved deeper, testing various amino acids to determine their effects on food intake. They identified three specific amino acids—glutamine, lysine, and threonine—that caused a pronounced aversion to protein consumption. Notably, when the mice were given food lacking these amino acids, their food intake returned to normal levels.
This led to the hypothesis that the aversion was linked to ammonia production during protein metabolism. Ammonia is a toxic byproduct that the body must detoxify, a process that requires additional water and leads to increased urination. Consequently, the researchers speculated that the mice adjusted their protein intake based on their ability to manage ammonia levels.
Understanding the Gut-Brain Signaling Axis
The study also explored how the body senses ammonia production. The researchers pinpointed the duodenum, a section of the small intestine, as the area where ammonia levels are detected. They identified a specific receptor on intestinal cells that plays a crucial role in this process. Mice lacking this receptor showed no aversion to protein-rich foods, while activating the receptor led to a significant decrease in their food intake.
The research extended to the brain, revealing that two regions in the brainstem, the area postrema and the nucleus tractus solitarius, were involved in this signaling pathway. These areas are known to regulate satiety and nausea, and their connection to the gut’s ammonia detection provides insight into how the body communicates its needs during recovery.
Dr. Joseph Luchsinger, a co-first author of the study, highlighted the broader implications of this research, particularly in understanding eating behaviors in psychiatric illnesses like anorexia. “How and why we choose to eat is really poorly understood,” he stated, emphasizing the need for further exploration in this area.
The findings raise important questions about dietary recommendations for individuals recovering from illness. Previous clinical trials suggested that high-protein diets did not improve outcomes for patients recovering from critical illnesses and may even have adverse effects. The current study, while conducted in mice, indicates the necessity for revised dietary guidelines that could lead to better recovery strategies.
Moving forward, the research team intends to investigate how varying protein sources and amino acid compositions could influence recovery outcomes across different physiological and disease states. Dr. Jaschke noted that these insights could be particularly relevant for individuals with urea cycle disorders, as well as for those with conditions marked by suppressed appetite, such as anorexia or cancer cachexia.
In conclusion, this research offers a novel perspective on the relationship between gut health and dietary preferences during recovery from illness. As the team continues to explore these mechanisms, the hope is to develop therapeutic approaches that will support patients in their recovery journeys.
-

 Top Stories1 month ago
Top Stories1 month agoUrgent Update: Tom Aspinall’s Vision Deteriorates After UFC 321
-
 Health1 month ago
Health1 month agoMIT Scientists Uncover Surprising Genomic Loops During Cell Division
-

 Science4 weeks ago
Science4 weeks agoUniversity of Hawaiʻi Joins $25.6M AI Project to Enhance Disaster Monitoring
-

 Top Stories1 month ago
Top Stories1 month agoAI Disruption: AWS Faces Threat as Startups Shift Cloud Focus
-
 Science2 months ago
Science2 months agoTime Crystals Revolutionize Quantum Computing Potential
-

 World2 months ago
World2 months agoHoneywell Forecasts Record Business Jet Deliveries Over Next Decade
-

 Entertainment1 month ago
Entertainment1 month agoDiscover the Full Map of Pokémon Legends: Z-A’s Lumiose City
-

 Top Stories2 months ago
Top Stories2 months agoGOP Faces Backlash as Protests Surge Against Trump Policies
-

 Entertainment2 months ago
Entertainment2 months agoParenthood Set to Depart Hulu: What Fans Need to Know
-

 Politics2 months ago
Politics2 months agoJudge Signals Dismissal of Chelsea Housing Case Citing AI Flaws
-

 Sports2 months ago
Sports2 months agoYoshinobu Yamamoto Shines in Game 2, Leading Dodgers to Victory
-
 Health2 months ago
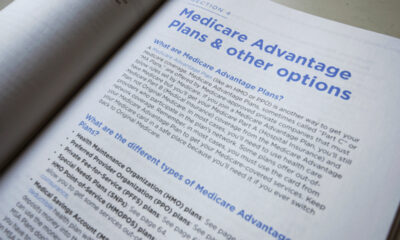
Health2 months agoMaine Insurers Cut Medicare Advantage Plans Amid Cost Pressures









