Health
Scientists Illuminate Seasonal Affective Disorder’s Biological Roots

As the days shorten and the temperatures drop, many individuals experience a profound shift in mood, a phenomenon known as seasonal affective disorder (SAD). Recent research has begun to uncover the biological mechanisms behind this condition, which was formally recognized by mental health professionals in the 1980s. Dr. Cathy Wyse, a chancellor’s research fellow at the University of Edinburgh, highlights significant advances in understanding how seasonal changes affect human physiology and mood.
Historically, the connection between seasons and emotional well-being has been noted for centuries. The Yellow Emperor’s Classic of Medicine, a Chinese text dating back to approximately 300 BC, advised individuals to adapt their behaviors with the changing seasons by retreating early in winter and maintaining a subdued mental state. This ancient wisdom aligns with modern findings that suggest seasonal variations in mood are deeply embedded in our biology.
Research utilizing large-scale databases, such as the UK Biobank, has provided new insights into how seasonal patterns influence thousands of individuals over extended periods. Dr. Wyse emphasizes that the most significant discovery in recent years is understanding that these mood changes are likely endogenous, meaning they are a natural part of our physiological makeup.
SAD is characterized by a predictable seasonal pattern, with symptoms typically emerging in autumn or winter and subsiding in spring. Individuals experiencing SAD often report increased sleep, lethargy, and a craving for carbohydrates. The triggers for these mood shifts are still under investigation, but there is a consensus that reduced daylight plays a crucial role. Light serves as a vital regulator of our internal body clock, impacting hormone release, alertness, and overall mood.
Without adequate exposure to natural light, particularly when excessive artificial light is present in the evenings, these biological rhythms can become misaligned. Dr. Wyse and her colleagues are also exploring seasonal effects in bipolar disorder, where symptoms often correlate with seasonal changes. “We suspect that people with bipolar disorder may be very sensitive to light and seasonal cues, triggering their symptoms,” she stated.
Beyond clinical depression, many individuals experience a milder form of seasonal mood variation known as subsyndromal SAD or the “winter blues.” In the UK, it is estimated that one in five people are affected by this seasonal dip, while only about 2% are diagnosed with full-blown SAD.
The implications of seasonal biology extend beyond mood. Recent studies indicate significant fluctuations in the expression of over 4,000 protein-coding genes in blood cells and fat, as well as changes in blood composition throughout the year. An analysis of four years’ worth of sleep data from the UK Biobank, involving half a million participants, revealed that individuals tend to sleep longer in winter but also experience poorer sleep quality compared to summer months.
Despite the natural occurrence of these seasonal changes, societal expectations often compel individuals to maintain their usual routines. While hibernation may not be a viable option, light therapy remains the most effective treatment for SAD, with timing and dosage being critical factors for success. For those unable to commit to a daily session in front of a light box, exposure to natural sunlight can serve as a powerful alternative.
Research on Amish communities in the United States, who spend more time outdoors and are less exposed to bright artificial light in the evenings, has shown some of the lowest rates of SAD among Caucasian populations. In contrast, the prevalence of SAD in New York is approximately 4.7%. Natural light exposure in the morning plays a key role in realigning the circadian clock and suppressing melatonin, a hormone that can contribute to grogginess. Furthermore, studies indicate that an hour of blue-enriched light can enhance reaction times more effectively than the equivalent of two cups of coffee.
While light therapy is crucial, it is not the sole solution. Cognitive behavioural therapy tailored for SAD has proven to be as effective as light therapy, assisting individuals in reframing their perceptions of winter rather than merely managing symptoms.
As winter approaches, individuals can take proactive steps to mitigate the effects of seasonal mood changes. Engaging with morning sunlight, utilizing light boxes, maintaining regular sleep patterns, and planning enjoyable winter activities can significantly improve one’s outlook during darker months.
For those experiencing persistent mood, sleep, or motivation issues that interfere with daily life, seeking professional help is essential. SAD is treatable, and support is available through various organizations. In the UK, Mind can be reached at 0300 123 3393, while Childline offers assistance at 0800 1111. In the United States, individuals can contact Mental Health America at 988 or visit 988lifeline.org. In Australia, resources are available through Beyond Blue at 1300 22 4636, Lifeline at 13 11 14, and MensLine at 1300 789 978.
By understanding the biological underpinnings of seasonal affective disorder and implementing effective strategies, individuals can better navigate the challenges posed by the winter months.
-

 Top Stories1 month ago
Top Stories1 month agoUrgent Update: Tom Aspinall’s Vision Deteriorates After UFC 321
-
 Health1 month ago
Health1 month agoMIT Scientists Uncover Surprising Genomic Loops During Cell Division
-

 Science4 weeks ago
Science4 weeks agoUniversity of Hawaiʻi Joins $25.6M AI Project to Enhance Disaster Monitoring
-

 Top Stories1 month ago
Top Stories1 month agoAI Disruption: AWS Faces Threat as Startups Shift Cloud Focus
-
 Science2 months ago
Science2 months agoTime Crystals Revolutionize Quantum Computing Potential
-

 World2 months ago
World2 months agoHoneywell Forecasts Record Business Jet Deliveries Over Next Decade
-

 Entertainment1 month ago
Entertainment1 month agoDiscover the Full Map of Pokémon Legends: Z-A’s Lumiose City
-

 Top Stories2 months ago
Top Stories2 months agoGOP Faces Backlash as Protests Surge Against Trump Policies
-

 Entertainment2 months ago
Entertainment2 months agoParenthood Set to Depart Hulu: What Fans Need to Know
-

 Politics2 months ago
Politics2 months agoJudge Signals Dismissal of Chelsea Housing Case Citing AI Flaws
-

 Sports2 months ago
Sports2 months agoYoshinobu Yamamoto Shines in Game 2, Leading Dodgers to Victory
-
 Health2 months ago
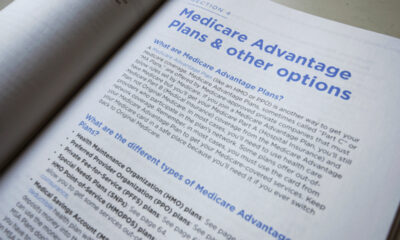
Health2 months agoMaine Insurers Cut Medicare Advantage Plans Amid Cost Pressures







